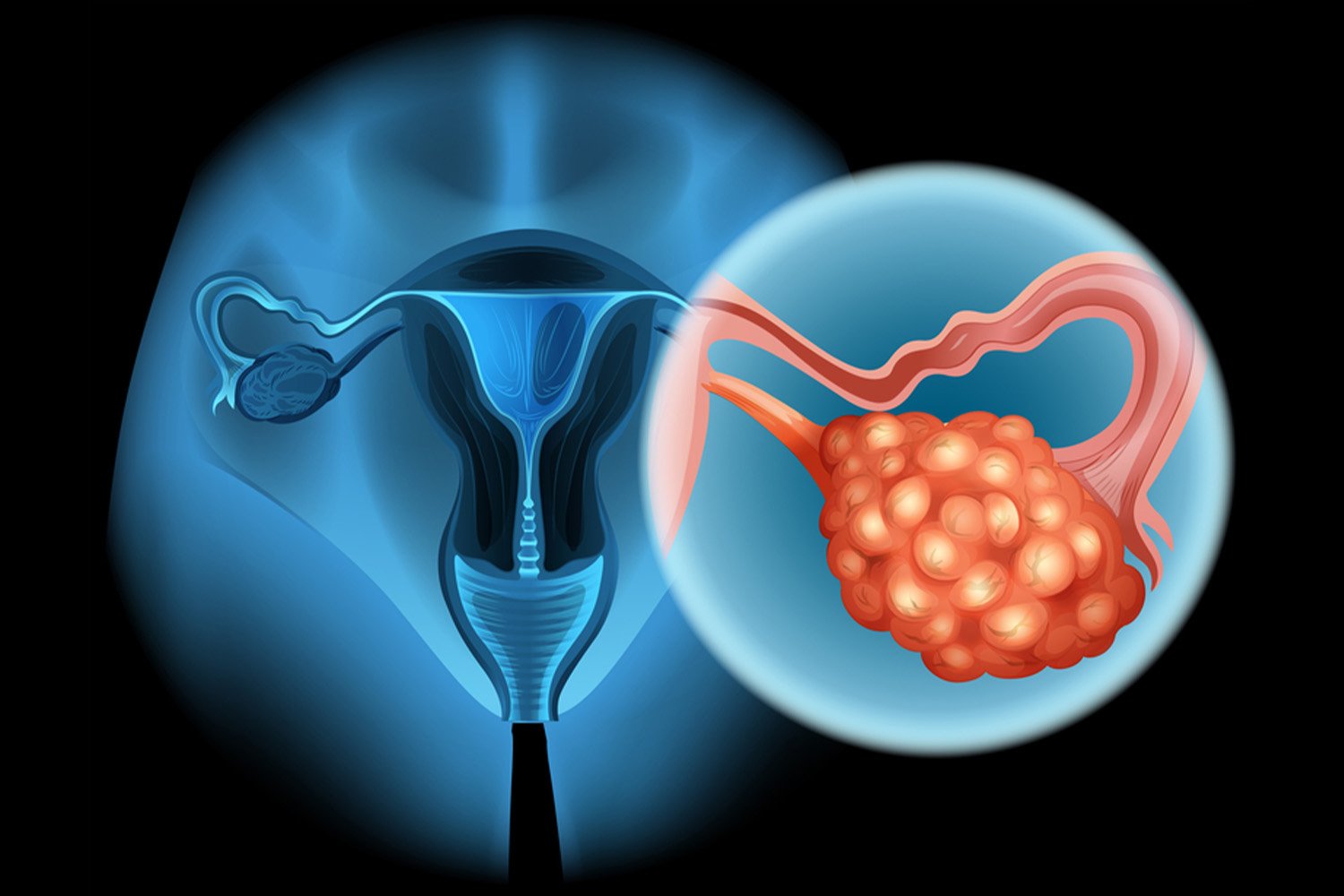
Gynecological cancers encompass a range of malignancies affecting the female reproductive system, including ovarian, cervical, uterine, vaginal, and vulvar cancers. While lifestyle and environmental factors contribute significantly to their development, understanding the role of hereditary risk factors is crucial in both prevention and treatment strategies.
Inherited genetic mutations play a pivotal role in predisposing individuals to gynecological cancers. These mutations can be passed down through families and significantly increase the likelihood of developing these malignancies. While environmental factors such as smoking, obesity, and infections like HPV also contribute to the risk, understanding the genetic component is essential for effective management.
Dr. Gopal Sharma, a distinguished specialist in gynecological cancers, emphasizes the importance of recognizing hereditary risk factors in clinical practice. Identifying individuals with genetic predispositions allows for targeted screening, early detection, and personalized treatment plans.
Among the most notable hereditary risk factors are mutations in the BRCA1 and BRCA2 genes. These genes are associated with an increased risk of breast and ovarian cancers. Women carrying BRCA1 mutations have a significantly higher risk of developing ovarian cancer, while BRCA2 mutations increase the risk of both ovarian and breast cancers.
Lynch syndrome, another hereditary condition, predisposes individuals to various cancers, including endometrial and ovarian cancers. It is caused by mutations in genes responsible for DNA repair, such as MLH1, MSH2, MSH6, and PMS2. Women with Lynch syndrome face a substantially elevated risk of developing gynecological cancers over their lifetime.
Furthermore, hereditary non-polyposis colorectal cancer (HNPCC), also known as Lynch syndrome, significantly increases the risk of endometrial and ovarian cancers. Individuals with HNPCC mutations have an up to 12% lifetime risk of developing endometrial cancer and a 9% risk of ovarian cancer.
Understanding one’s genetic predisposition to gynecological cancers empowers individuals to make informed decisions regarding their health. Genetic counseling and testing play a crucial role in assessing the risk and guiding preventive measures. Screening protocols, including transvaginal ultrasound, CA-125 blood tests, and pelvic exams, are recommended for high-risk individuals to facilitate early detection and intervention.
Dr. Gopal Sharma emphasizes the importance of a multidisciplinary approach in managing hereditary risk factors for gynecological cancers. Collaborative efforts between gynecologists, oncologists, genetic counselors, and other healthcare professionals ensure comprehensive care tailored to individual needs.
In addition to proactive screening measures, lifestyle modifications, and risk-reducing surgeries may be recommended for high-risk individuals. Prophylactic removal of the ovaries and fallopian tubes (salpingo-oophorectomy) significantly reduces the risk of ovarian cancer in women with BRCA mutations.
In conclusion, hereditary risk factors play a significant role in the development of gynecological cancers. Understanding one’s genetic predisposition empowers individuals to take proactive steps toward prevention and early detection. Through collaborative efforts and personalized interventions, we can mitigate the impact of hereditary factors on women’s health and improve outcomes in gynecological cancer management.